
In recent years, the incidence of fractures has increased with the aging of the population, and the global attention to fracture prevention and treatment has been greatly increased. Vitamin D is an indispensable nutrient in human life and is mainly involved in the regulation of calcium and phosphorus in the body as well as bone metabolism. Vitamin D is now widely recommended for use in the general population as an important means of promoting bone health. Relevant data show that from 1999 to 2012, the use of vitamin D supplements among adults in the United States increased from 5.1% to 19%.
However, different studies have produced conflicting results as to whether vitamin D supplements actually prevent fractures. Recently, the New England Journal of Medicine (NEJM) published the results of an analysis of the heavyweight study VITAL, which confirmed that high-dose vitamin D3 supplementation (2000 IU/day) did not significantly reduce the risk of fracture compared to placebo in a general healthy middle-aged/older adult population not associated with vitamin D deficiency, low bone mass or osteoporosis.
The paper highlights that previous analyses from the VITAL study have confirmed that taking higher doses of vitamin D does not prevent heart disease, cancer or memory loss. The findings of this current analysis again overturn previous dogma and question the value of testing vitamin D levels in routine blood tests and the current recommendations for vitamin D supplementation in different guideline consensus.
Translated with www.DeepL.com/Translator (free version)
Vitamin D supports bone health and improves bone mineralization levels by promoting calcium absorption in the intestine, reducing secondary hyperparathyroidism, and decreasing bone turnover levels. In addition, extrarenal activation of vitamin D receptors in bone and 1,25-dihydroxyvitamin D is also associated with the formation of osteogenic progenitor cells, further suggesting an important role for vitamin D in bone formation.
In 2011, the Institute of Medicine (IOM) recommended a daily dietary intake of 600-800 IU of vitamin D for adults, corresponding to a total level of at least 20 ng/ml of 25-hydroxyvitamin D (the primary form of vitamin D in the body) (about one-third of the global population does not meet this standard for serum 25-hydroxyvitamin D levels). In addition, other societies and organizations recommend a daily intake of at least 800 to 2000 IU of vitamin D for adults ≥50 years of age to achieve serum 25-hydroxyvitamin D levels of at least 30 ng/ml.
However, previous randomized, controlled trials exploring the effects of vitamin D supplementation on fractures have yielded inconsistent analyses (including beneficial, no effect, or even harmful). In addition, to date, there has been a lack of large, randomized controlled trials evaluating the preventive effects of daily vitamin D supplementation alone (not combined with calcium) in fractures.
The VITAL study was a randomized, controlled trial designed to evaluate the primary prevention of cancer and cardiovascular disease with vitamin D3 supplementation (cholecalciferol, 2000 IU/day) and n-3 fatty acids (Omacor, 1 g/day) in men ≥50 years of age and women ≥55 years of age in the United States.
In an ancillary study to the VITAL study, researchers analyzed whether vitamin D3 supplementation compared to placebo would reduce the risk of fractures (subjects without vitamin D deficiency, low bone mass, or osteoporosis). The primary endpoints analyzed were overall fractures, non-vertebral fractures, and hip fracture events.
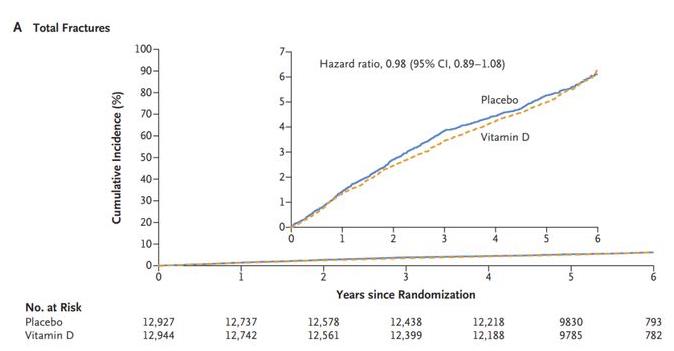
The study showed that a total of 25,871 subjects (50.6% female; 20.2% black) were included in the final analysis. During a median follow-up of 5.3 years, a total of 1,551 subjects had 1,991 fracture events. Of these, a total of 769 fractures occurred in 12927 subjects in the vitamin D3 supplementation group; 782 fractures occurred in 12944 subjects in the placebo group.
The results of the analysis showed that vitamin D3 supplementation did not have an effect on overall fractures (HR=0.98; 95% CI: 0.89-1.08; P=0.70), nonvertebral fractures (HR=0.97; 95% CI: 0.87-1.07; P=0.50), and hip fractures (HR=1.01; 95% CI: 0.70-1.47; P=0.50) in subjects compared with placebo. 1.47; P=0.96) had a significant effect on the risk of occurrence.
Translated with www.DeepL.com/Translator (free version)
Overall, the results of the current large randomized, controlled trial suggest that taking vitamin D3 supplementation (2000 IU/day, not combined with calcium) did not significantly reduce the risk of fracture in the general US adult population (i.e., without vitamin D deficiency, low bone mass, or osteoporosis) compared with placebo.
In addition, a post hoc analysis of the study showed that even subjects who also took calcium (about 20%) and those with low blood vitamin D levels (<12 ng/ml) did not show a significant benefit in terms of reduced risk of fracture occurrence.
The study authors emphasize that for most people, spending more time outdoors doing physical activity and maintaining a healthy diet is expected to provide a greater benefit than taking vitamin D supplements. Although vitamin D is important for bone health, it does not mean that the more vitamin D the body takes, the better. Nor should one hope to prevent major diseases by taking vitamin D supplements.
However, the study authors also emphasized that more research is needed to determine whether other high-risk groups may benefit from vitamin D supplements.
Translated with www.DeepL.com/Translator (free version)